|
Pain Med. 2020 Feb 1;21(2):e139-e145. doi: 10.1093/pm/pnz219.
Association Between Chiropractic Use and Opioid Receipt Among Patients with Spinal Pain: A Systematic Review and Meta-analysis. Corcoran KL1,2, Bastian LA2,3, Gunderson CG2,3, Steffens C2, Brackett A4, Lisi AJ1,2.Author information Abstract OBJECTIVE: To investigate the current evidence to determine if there is an association between chiropractic use and opioid receipt. DESIGN: Systematic review and meta-analysis. METHODS: The protocol for this review was registered on PROSPERO (CRD42018095128). The MEDLINE, PubMed, EMBASE, AMED, CINAHL, and Web of Science databases were searched for relevant articles from database inception through April 18, 2018. Controlled studies, cohort studies, and case-control studies including adults with noncancer pain were eligible for inclusion. Studies reporting opioid receipt for both subjects who used chiropractic care and nonusers were included. Data extraction and risk of bias assessment were completed independently by pairs of reviewers. Meta-analysis was performed and presented as an odds ratio with 95% confidence interval. RESULTS: In all, 874 articles were identified. After detailed selection, 26 articles were reviewed in full, and six met the inclusion criteria. Five studies focused on back pain and one on neck pain. The prevalence of chiropractic care among patients with spinal pain varied between 11.3% and 51.3%. The proportion of patients receiving an opioid prescription was lower for chiropractic users (range = 12.3-57.6%) than nonusers (range = 31.2-65.9%). In a random-effects analysis, chiropractic users had a 64% lower odds of receiving an opioid prescription than nonusers (odds ratio = 0.36, 95% confidence interval = 0.30-0.43, P < 0.001, I2 = 92.8%). CONCLUSIONS: This review demonstrated an inverse association between chiropractic use and opioid receipt among patients with spinal pain. Further research is warranted to assess this association and the implications it may have for case management strategies to decrease opioid use. © 2019 American Academy of Pain Medicine. All rights reserved. For permissions, please e-mail: [email protected]. KEYWORDS: Analgesic; Chiropractic; Low Back Pain; Meta-analysis; Neck Pain; Opioid; Systematic Review PMID:31560777 DOI: 10.1093/pm/pnz219 A study exploring the prevalence of Extremity Pain of Spinal Source (EXPOSS)
Richard Rosedale,Ravi Rastogi,Josh Kidd,Greg Lynch,Georg Supp &Shawn M Robbins Published online: 02 Sep 2019 ABSTRACT Objectives: To investigate the proportion of patients that present with isolated extremity pain who have a spinal source of symptoms and evaluate the response to spinal intervention. Methods: Participants (n = 369) presenting with isolated extremity pain and who believed that their pain was not originating from their spine, were assessed using a Mechanical Diagnosis and Therapy differentiation process. Numerical Pain Rating Scale, Upper Extremity/Lower Extremity Functional Index and the Orebro Questionnaire were collected at the initial visit and at discharge. Global Rating of Change outcomes were collected at discharge. Clinicians provided MDT ‘treatment as usual’. A chi-square test examined the overall significance of the comparison within each region. Effect sizes between spinal and extremity source groups were calculated for the outcome scores at discharge Results: Overall, 43.5% of participants had a spinal source of symptoms. Effect sizes indicated that the spinal source group had improved outcomes at discharge for all outcomes compared to the extremity source group. Discussion: Over 40% of patients with isolated extremity pain, who believed that their pain was not originating from the spine, responded to spinal intervention and thus were classified as having a spinal source of symptoms. These patients did significantly better than those whose extremity pain did not have a spinal source and were managed with local extremity interventions. The results suggest the spine is a common source of extremity pain and adequate screening is warranted to ensure the patients ́ source of symptoms is addressed. Best Core Stabilization for Anticipatory Postural Adjustment and Falls in Hemiparetic Stroke.6/12/2018
Arch Phys Med Rehabil. 2018 Feb 21. pii: S0003-9993(18)30116-3. doi: 10.1016/j.apmr.2018.01.027. [Epub ahead of print]
Best Core Stabilization for Anticipatory Postural Adjustment and Falls in Hemiparetic Stroke .Lee NG1, You JSH2, Yi CH3, Jeon HS3, Choi BS1, Lee DR4, Park JM5, Lee TH6, Ryu IT7, Yoon HS8.Author information Abstract OBJECTIVES:To compare the effects of conventional core stabilization and dynamic neuromuscular stabilization (DNS) on anticipatory postural adjustment (APA) time, balance performance, and fear of falls in chronic hemiparetic stroke. DESIGN:Two-group randomized controlled trial with pretest-posttest design. SETTING:Hospital rehabilitation center. PARTICIPANTS:Adults with chronic hemiparetic stroke (N=28). INTERVENTIONS:Participants were randomly divided into either conventional core stabilization (n=14) or DNS (n=14) groups. Both groups received a total of 20 sessions of conventional core stabilization or DNS training for 30 minutes per session 5 times a week during the 4-week period. MAIN OUTCOME MEASURES:Electromyography was used to measure the APA time for bilateral external oblique (EO), transverse abdominis (TrA)/internal oblique (IO), and erector spinae (ES) activation during rapid shoulder flexion. Trunk Impairment Scale (TIS), Berg Balance Scale (BBS), and Falls Efficacy Scale (FES) were used to measure trunk movement control, balance performance, and fear of falling. RESULTS:Baseline APA times were delayed and fear of falling was moderately high in both the conventional core stabilizationand DNS groups. After the interventions, the APA times for EO, TrA/IO, and ES were shorter in the DNS group than in the conventional core stabilization group (P<.008). The BBS and TIS scores (P<.008) and the FES score (P<.003) were improved compared with baseline in both groups, but FES remained stable through the 2-year follow-up period only in the DNS group (P<.003). CONCLUSIONS:This is the first clinical evidence highlighting the importance of core stabilization exercises for improving APA control, balance, and fear of falls in individuals with hemiparetic stroke. Copyright © 2018 American Congress of Rehabilitation Medicine. Published by Elsevier Inc. All rights reserved. KEYWORDS:Rehabilitation; Stroke PMID: 29476713 DOI: 10.1016/j.apmr.2018.01.027 Effects of Cervical Extension on Deformation of Intervertebral Disk and Migration of Nucleus Pulposus
Kim, Yoon-Ho et al. PM&R , Volume 9 , Issue 4 , 329 - 338 Abstract Background We theorized that active cervical extension should influence the position of the nucleus pulposus (NP) within the intervertebral disk (IVD) in the sagittal plane. Although several studies on the lumbar IVD have been conducted, there are no quantitative data for in vivo positional changes of the NP in the cervical IVD. Objective To evaluate the influence and mechanism of cervical extension on the deformation and migration of IVD and NP in the sagittal plane and understand underlying mechanisms of the extension maneuver. Design Asymptomatic subjects underwent magnetic resonance imaging while supine with their cervical spines in neutral and extended positions. Setting Academic medical center. Participants Ten young, healthy male participants (age range 19-30 years; mean 22.4 ± 1.64 years). Methods T2-weighted sagittal images from C3-C4 to C6-C7 of subjects in both neutral and extension positions were analyzed. Main Outcome Measurements Deformation of IVD and positional change of NP were quantified and compared between neutral and extension positions. Intersegmental angles between vertebrae, horizontal positions of anterior and posterior IVD and NP margins, IVD outer and inner heights, and sagittal morphology of NP were quantified and compared between the neutral and extension positions. Correlations between the measured parameters and segmental extension angle were also investigated. Results Anterior and posterior IVD margins moved posteriorly with respect to the vertebral body in extension. Both NP margins remained unchanged relative to the vertebral body but moved anteriorly with respect to the IVD. IVD outer and inner heights in the anterior region increased in extension, and morphological changes of the NP were less noticeable when compared with its relative migration within the IVD. Most of the intradiskal changes were linearly correlated with the segmental extension angle. Conclusions Cervical extension induces anterior migration of the NP away from the posterior disk margin and may have a clinical effect on diskogenic neck pain resulting from internal disk disruption. Level of Evidence Not applicable. JAMA. 2018 Mar 6;319(9):872-882. doi: 10.1001/jama.2018.0899.
Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial Krebs EE1,2, Gravely A1, Nugent S1, Jensen AC1, DeRonne B1, Goldsmith ES1,3, Kroenke K4,5,6, Bair MJ4,5,6, Noorbaloochi S1,2.Author information Abstract IMPORTANCE: Limited evidence is available regarding long-term outcomes of opioids compared with nonopioid medications for chronic pain. OBJECTIVE: To compare opioid vs nonopioid medications over 12 months on pain-related function, pain intensity, and adverse effects. DESIGN, SETTING, AND PARTICIPANTS: Pragmatic, 12-month, randomized trial with masked outcome assessment. Patients were recruited from Veterans Affairs primary care clinics from June 2013 through December 2015; follow-up was completed December 2016. Eligible patients had moderate to severe chronic back pain or hip or knee osteoarthritis pain despite analgesic use. Of 265 patients enrolled, 25 withdrew prior to randomization and 240 were randomized. INTERVENTIONS: Both interventions (opioid and nonopioid medication therapy) followed a treat-to-target strategy aiming for improved painand function. Each intervention had its own prescribing strategy that included multiple medication options in 3 steps. In the opioid group, the first step was immediate-release morphine, oxycodone, or hydrocodone/acetaminophen. For the nonopioid group, the first step was acetaminophen (paracetamol) or a nonsteroidal anti-inflammatory drug. Medications were changed, added, or adjusted within the assigned treatment group according to individual patient response. MAIN OUTCOMES AND MEASURES: The primary outcome was pain-related function (Brief Pain Inventory [BPI] interference scale) over 12 months and the main secondary outcome was pain intensity (BPI severity scale). For both BPI scales (range, 0-10; higher scores = worse function or pain intensity), a 1-point improvement was clinically important. The primary adverse outcome was medication-related symptoms (patient-reported checklist; range, 0-19). RESULTS: Among 240 randomized patients (mean age, 58.3 years; women, 32 [13.0%]), 234 (97.5%) completed the trial. Groups did not significantly differ on pain-related function over 12 months (overall P = .58); mean 12-month BPI interference was 3.4 for the opioid group and 3.3 for the nonopioid group (difference, 0.1 [95% CI, -0.5 to 0.7]). Pain intensity was significantly better in the nonopioid group over 12 months (overall P = .03); mean 12-month BPI severity was 4.0 for the opioid group and 3.5 for the nonopioid group (difference, 0.5 [95% CI, 0.0 to 1.0]). Adverse medication-related symptoms were significantly more common in the opioid group over 12 months (overall P = .03); mean medication-related symptoms at 12 months were 1.8 in the opioid group and 0.9 in the nonopioid group (difference, 0.9 [95% CI, 0.3 to 1.5]). CONCLUSIONS AND RELEVANCE: Treatment with opioids was not superior to treatment with nonopioid medications for improving pain-related function over 12 months. Results do not support initiation of opioid therapy for moderate to severe chronic back pain or hip or knee osteoarthritis pain. TRIAL REGISTRATION: clinicaltrials.gov Identifier: NCT01583985. PMID: 29509867 DOI: 10.1001/jama.2018.0899 DNS stands for Dynamic Neuromuscular Stabilization. DNS was developed by Professor Pavel Kolar of the Prague School of Rehabilitation at Charles University Motol Hospital in the Czech Republic. DNS is a system based on developmental kinesiology and human ontogenesis. Every human with a normally developing central nervous system activates the same sequence of movement, locomotor, patterns. These patterns are ideal with perfect joint centration (maximum bearing surface congruency) and co-activation of the agonist/antagonist musculature controlling the joint. These patterns are unlearned and are genetically programmed or pre-determined. DNS is concerned with activating these patterns to restore ideal biomechanics and human locomotion. A foundational concept in DNS is activation of the Intrinsic Spinal Stabilization System (ISSS) through the mechanism of Intra-Abdominal Pressure (IAP). When we have proper activation and descent of the diaphragm, concentric activity, we compress our viscera creating increased IAP pushing back against the trunk wall in all directions. Due to the increased IAP we have reactive eccentric activity of all of the components of the trunk and pelvic floor. This fixes/stabilizes the ISSS and makes the trunk an anchor for distal and proximal muscle pull from the extremities. This mechanism is pre-requisite for all other purposeful extremity movement to stabilize the trunk and prevent aberrant movement in the spine. This mechanism represents a global pattern of control that when working properly ensures the most efficient strategy for human locomotion
Spine (Phila Pa 1976). 1996 Nov 15;21(22):2640-50.
Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Hodges PW1, Richardson CA. This hallmark study shows the stabilization function of the trunk that is required preceding any purposeful movement of the extremities. The trunk functions as an anchor for muscle pull towards and away from the spine. This is governed by a global motor control pattern or strategy. When there is dysfunction in the motor control pattern (CNS) there is instability and aberrant movement in the spine. Dynamic Neuromuscular Stabilization (DNS) accesses and restores the ideal movement strategy/global motor control pattern. By: Julie Kulig, DC
Where has the year gone? It is almost December and the holiday season is in full swing! This is a wonderful time of the year but it’s also a time when our exercise regimen takes a backseat to our indulgences. Did you vow to exercise more this year? Or maybe you are already thinking of your soon to be New Year’s Resolutions. The time is now. The best answer to staying healthy is staying active. Exercise brings about the following myriad of benefits: Decreased risk of cardiovascular disease Weight control Decreased risk of Type 2 diabetes Decreased risk of osteoporosis (weight bearing/strengthening exercise) Decreased risk of certain types of cancer Decreased risk of falls Improved mood and outlook on life How can I get started you might ask? Well it’s as simple as getting outside and going on a brisk walk. Research suggests that brisk walking at a moderate-intensity can provide benefits for you. So, if you think you are not in shape enough to begin. Think again. DID YOU KNOW??? Most frail, older individuals gain benefit from exercise at least as much as younger people. !! If you have a chronic health condition- it is always important to talk to your doctor about beginning a safe program for you- But, the bottom line is: the health benefits far outweigh the risks of getting hurt. If you have questions feel free to ask Dr. Brad Kulig or myself, Dr. Julie Kulig. We are happy to provide you with advice on beginning an exercise regimen. References: "Physical Activity and Health." Centers for Disease Control and Prevention: Physical Activity and Health. Centers for Disease Control and Prevention, 04 June 2015. Web. 29 Nov. 2016. Johnston, Brian D. "Overview of Exercise." Merck Manuals Professional Edition. N.p., Oct. 2016. Web. 29 Nov. 2016. 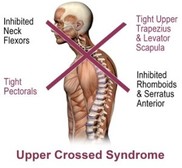 By: Julie Kulig, DC Do you know where your traps are? How about your upper trapezius? If you are shaking your head no right now- you are activating this muscle. It’s the muscle at the base of your neck and the top of your shoulders where we commonly here people say “that’s where I hold my stress.” This muscle is also commonly over-activated in those with upper crossed syndrome. Upper crossed syndrome is a muscle imbalance syndrome. It is most common in those who sit for the majority of the day. Think about it, how often do you sit at work each day? How often do you sit at home? We are creatures that are born to move. Chronic prolonged sitting leads to joint decentration. Which leads to upper crossed syndrome which leads to further joint decentration. Which came first? The chicken or the egg. It’s a perpetual cycle. Joint centration or a neutral joint position occurs when joint surface congruency and muscles that support the joint are at their optimal position throughout the range of motion and thus are able to produce varying forces according to the required skill. The centrated joint allows for optimal load transference of muscular forces across the joint and along the kinetic chain, with minimal mechanical stress on the passive structures such as ligaments, capsule, cartilage, and joint surfaces. Upper crossed syndrome is a muscle imbalance pattern located at the head and shoulder regions. It is most commonly found in individuals who work at a desk or sit for the majority of the day. Upper crossed syndrome leads to tightness in your upper trapezius and levator scapula, along with your suboccipital musculature at the base of your skull. It “crosses” with tightness in the pectoralis major and minor on your chest. It leads to weakness of your deep neck flexors that “crosses” with weakness in your middle and lower trapezius, rhomboids, and serratus anterior. So we are left with a jutted chin and what some people may call a “hump” in the upper back. It also leads to dysfunction and joint decentration at the following joints: atlanto-occipital joint, cervicothoracic junction, T4-T5 segment and the glenohumeral joint. In this postural presentation the plumb line of our head becomes forward of the plumb line in our necks. This puts an anterior load on the cervical intervertebral discs, putting them at risk for a disc injury such as a disc bulge and/or disc herniation, which may result in serious neurological consequences. This syndrome can also lead to headaches, temporal-mandibular joint dysfunction, shoulder problems, pain in the neck, and upper back, along with increased load on the passive structures in our spine which may have an impact on the degeneration of our joints at a more rapid pace. This is due to the decentrated joints that occur from this muscular imbalance syndrome. Because of these problems, it is important for the issue to be addressed. We take the time at our office to assess joint function, look for any muscular imbalances, and work to strengthen and stabilize weak muscles, along with stretching the appropriate muscle that may be short. We also encourage activity and becoming a more active individual. Be active. Move well. Live well. www.ButlerDC.Com With fall sports upon us, here is an interesting article on how to increase athletic performance:
A non-randomized experimental feasibility study into the immediate effect of three different spinal manipulative protocols on kicking speed performance in soccer players. -Chiropr Man Therap. 2015 Jan 13; 23 (1) There were 4 groups of 10: group 1: SI joint manipulation group 2: lumbar spine manipulation group 3: combination of lumbar spine and SI joint manipulation group 4: laser result: significant increase in kicking speed/ performance in the manipulation groups with the best being the combination group 3. Moral of the story: to improve performance in your sport - come get adjusted. #movewelllivewell #ButlerChiropractic |
Archives
February 2020
Categories |
HoursMWF: 9am - 6pm
T: 10am-5pm R: 9am-5pm |
Telephone814-355-0032
|
Email
|
